What is MCTP?
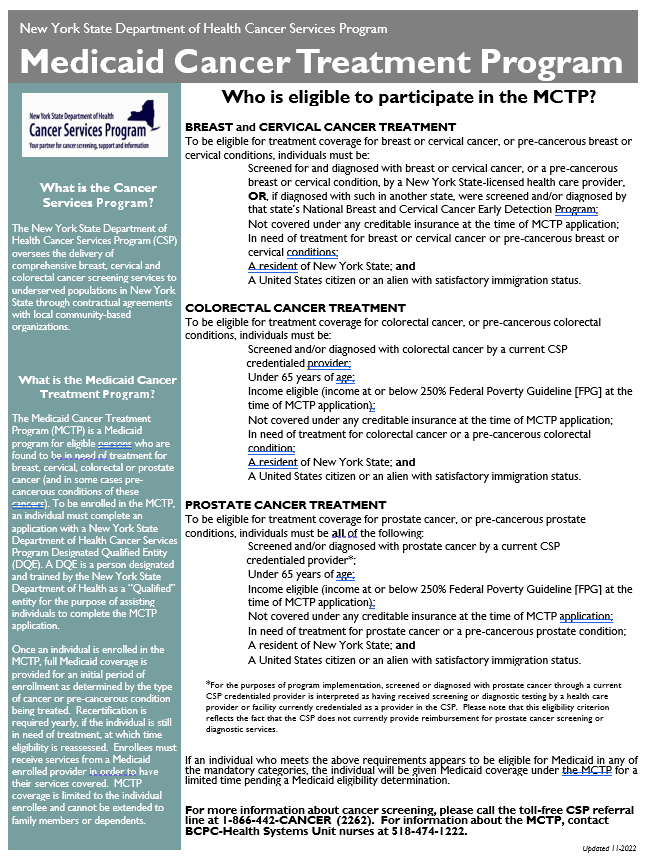
The Medicaid Cancer Treatment Program (MCTP) is a Medicaid program for eligible persons who are found to be in need of treatment for breast, cervical, colorectal or prostate cancer (and in some cases pre- cancerous conditions of these cancers). To be enrolled in the MCTP, an individual must complete an application with a New York State Department of Health Cancer Services Program Designated Qualified Entity (DQE). A DQE is a person designated and trained by the New York State Department of Health as a “Qualified” entity for the purpose of assisting individuals to complete the MCTP application.
Once an individual is enrolled in the MCTP, full Medicaid coverage is provided for an initial period of enrollment as determined by the type of cancer or pre-cancerous condition being treated. Recertification is required yearly, if the individual is still in need of treatment, at which time eligibility is reassessed. Enrollees must receive services from a Medicaid enrolled provider in order to have their services covered. MCTP coverage is limited to the individual enrollee and cannot be extended to family members or dependents.
DO I QUALIFY, AND IF SO, HOW CAN I ENROLL?
Our case manager can help. Fill out the “request information” form, check “MCTP” and she will contact you.